70 year old male with c/o sob cough since 10 days and fever since 5 days
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
CONSENT WAS GIVEN BY BOTH PATIENT AND ATTENDERS
Chief complaints
A 70 year old male came with Chief complaints of
SOB since 10 days
Cough since 10 days
Fever since 5 days
History of present illness
Patient was apparently asymptomatic 10 days back then he developed Shortness of breath which was of grade II ( MMRC ) associated with wheeze , aggravated on exertion , relieved on taking rest . complaints of cough since 10 days , non productive ( dry ) , aggravated on exposure to cool air .no c/o orthopnea , no PND . no c/o chest pain , chest tightness , hemoptysis , palpitations . c/o fever since 5 days which is of low grade , evening rise of temperature present , chills present , relieved on medication
Complaints of weight loss since 10 days
Complaints of Loss of appetite since 10 days
History of similar complaints in past 20 years back and seasonal variation present
Using local medication on and off
History of hospitalization for similar complaints 6 years back
H/o inhaler usage 6 years back for 1 year ( not using now )
No h/o TB in past
H/o DM II from 6 years on medication T. METFORMIN 500 mg
N/k/c/o HTN , CAD, Epilepsy , thyroid disorders
GENERAL PHYSICAL EXAMINATION
Patient is conscious coherent cooperative moderately built and nourished
No Pallor Icterus Clubbing Cyanosis Edema
Vitals :
PR : 73 bpm
BP : 110/70 mmHg
RR : 20 CPM
Temperature :
Spo2 : 98 %
GRBS :
SYSTEMIC EXAMINATION
CVS : S1 S2 +
CNS : NO focal neurological deficits
Per abdomen : soft non tender
URT :
Nose : no DNS
Oral cavity : poor dentition , normal oral hygiene
Posterior pharyngeal wall : normal
LRT
Inspection
Shape of chest elliptical
B/l symmetrical
Trachea central
Chest movements - equal on both sides
Drooping of shoulders on right side wasting of muscles +
Suprascapular hallowness present on both sides
Infraclavicular shallowness absent
Usage of accessory muscles of respiration present
No kyphosis and scoliosis
No scars and sinusis engorged veins and visible pulsations
Palpation
No local rise of temperature
No tenderness
All inspectory findings are confirmed
Trachea - central
Chest movements equal on both sides
Apex beat present in left 5 intercoastal space 2.5 cm medial to midclavicular line
VF equal on both sides
Diameters :
Transverse : 26 cm
Antero postero : 22 cm
Circumference : 82 cm
On percussion : resonant in all areas
On auscultation : BAE +
B/L ronchi + in ISA , IAA , MA , ICA , infra SA
B/L fine crepts + in IAA , Infra SA , ISA
Provisional Diagnosis
Acute exacerbation of COPD with type 2 DM
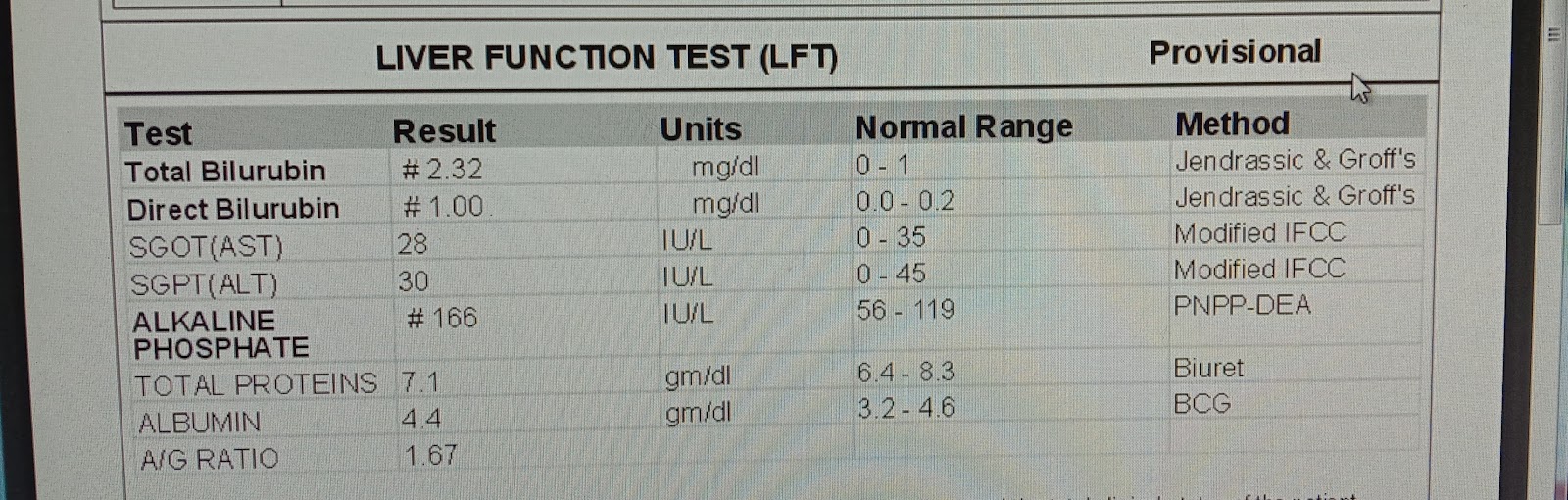
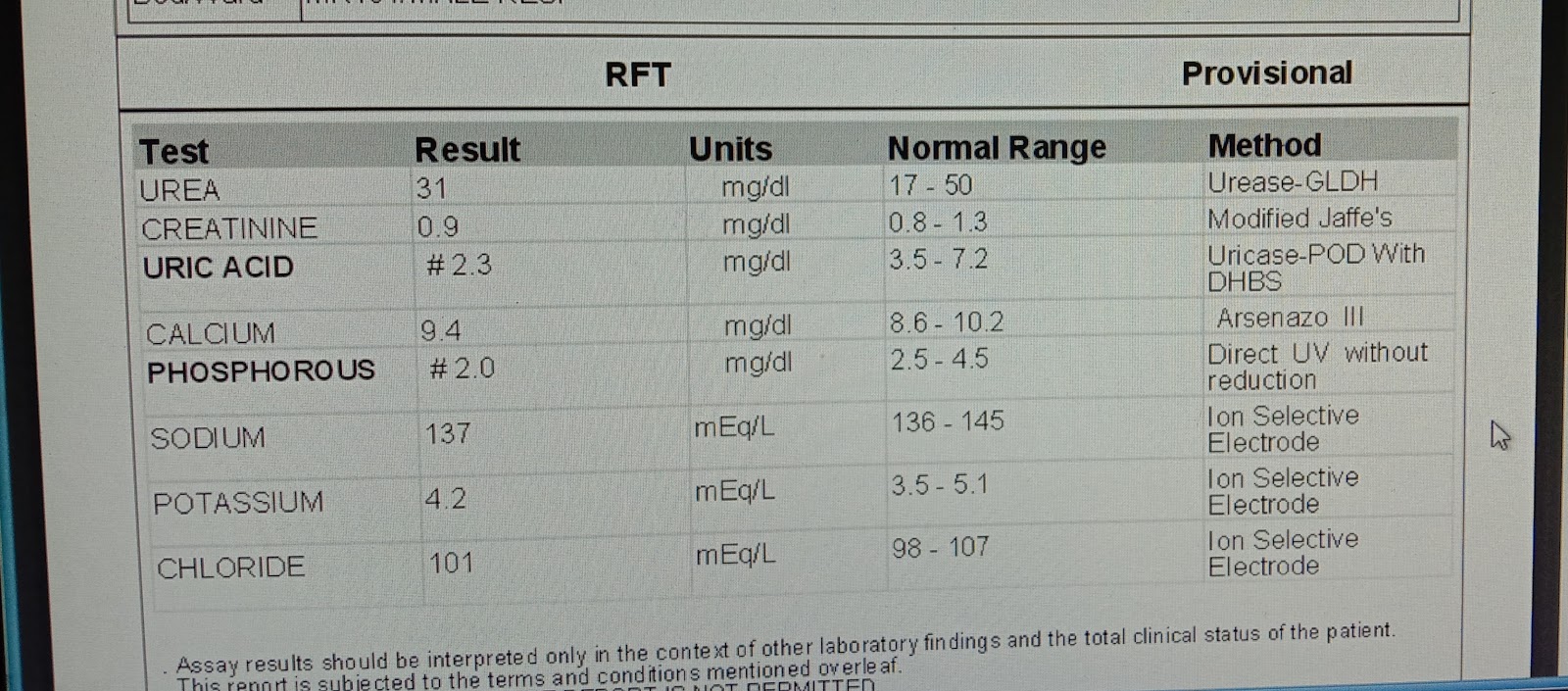
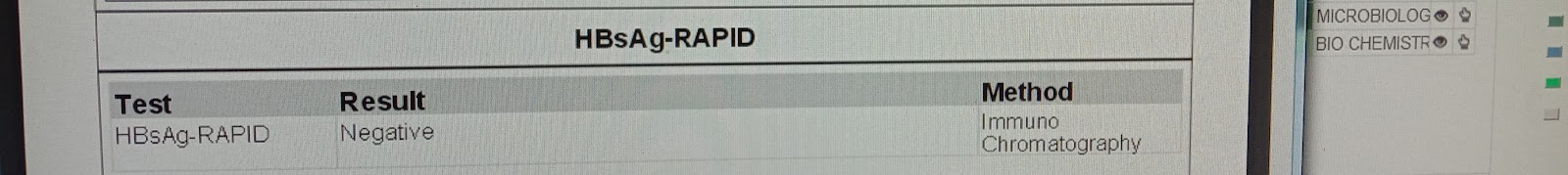
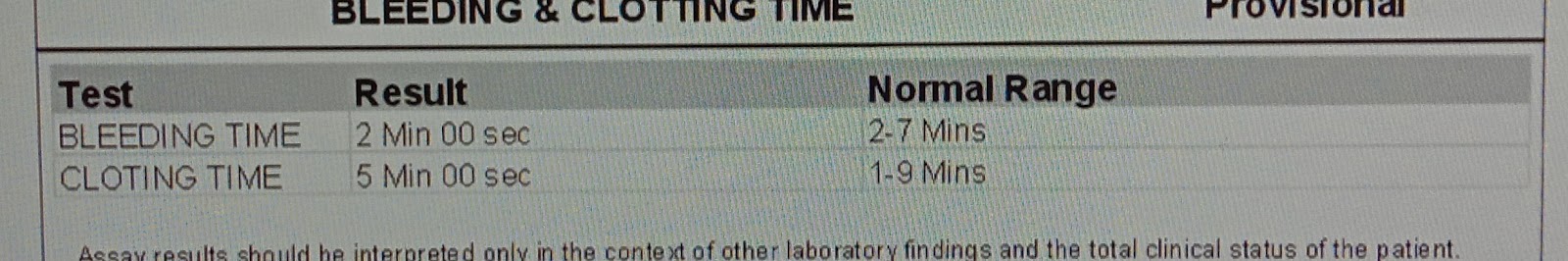
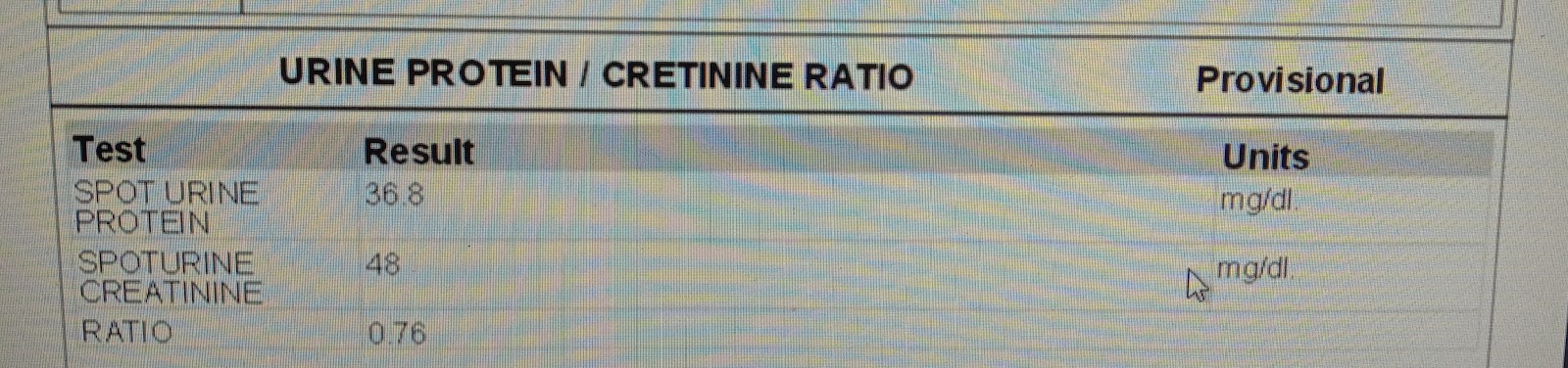
Investigations
Treatment
INJ PIPTAZ 4.5 gm IV TID
INJ LINEZOLID 600 mg IV BD
INJ PAN 40 mg IV OD BBF
INJ HUMAN ACTRAPID S/C TID
6u.........6u...........4u
INJ NPH SC BD
4u..........x..........4u
Nebulization with IPRAVENT 6th hrly
With BUDECORT 12th hrly
Tab METFORMIN 500mg PO /BD
Tab ACEBROPHYLLINE 100 mg PO OD
T PCM 650 PO TID
Syp GRYLINCTUS 2 tbs PO TID
Tab MONTEK LC PO Hs






























Comments
Post a Comment