A 43 year old male came with complaints of abdominal distension since 3 days complaints of bilateral pedal edemas in 3 days
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
CONSENT WAS GIVEN BY BOTH PATIENT AND ATTENDERS
A 43 year old male came with
complaints of abdominal distension since 3 days
complaints of bilateral pedal edemas in 3 days
complaint of fever since 7 days
HISTORY OF PRESENT ILLNESSS : -
Patient was apparently asymptomatic 7 days back then he developed fever which was sudden in onset gradually progressive , low grade not associated with cough and cold .
History of abdominal distension since 3 days which is insidious in onset gradually progressed to present size .
History of bilateral pedal edema since 3 days insidious in onset gradually progressive in nature , aggravated on standing or working relieved on rest
History of melena present , 1 month back for a week , resolved on its own
History of vomiting one episode which is non bilious, non blood stained, non projectile in nature one month back
History of loss of consciousness 2 days back not associated with seizures
No h/o paina broken , loose stools , constipation , shortness of breath , palpitations
Patient had a history of fall 10 days back
He didnt gain consciousness for 5 days
And for 3 days he remained in that area where he fell and no one noticed him his attenders didnt found him for 3 days and a shepard found him in woods and then the attenders took him to nearer hospital and found that he s having low sugars (ie due to 3 days of starvation ?)
After that he developed jaundice , abdominal distention and pedal edema
He is a chronic alcoholic since 20 years and daily he will take about 90- 180 ml of alcohol the last time he dank was 13 days back and when ever he stopped he will experience severe sweating , shiviring , and generalized weakness
Patient was conscious,coherent cooperative poorly build and nourished
Pallor : present
Icterus: present
clubbing: absent
cyanosis: absent
Lymphadenopathy: absent
Edema : present
SYSTEMIC EXAMINATION
Per abdomen :
On Inspection :
Abdomen is distended
Flanks are full
Umbilicus : inverted and smilely
Scars were present below umbilicus
Palpation :
No local raise of temperature
Abdomen is tense
abdominal girth : 93 cms
On percussion
A dull note is heard
On auscultation
Decreased bowel sounds are heard
Respiratory system
On inspection :
Shape of chest is normal
Looks like symmetrically expanding
No scars and sinuses
Trachea is central
On palpation :
no local raise of temperature or tenderness
All inspectory findings were confirmed
Chest is symmetrically expanding On both sides
On percussion
Purssion note is same on both sides
On auscultation :
Bilateral air entry was present
Normal vesicular breath sounds were heard
CVS :
S1 S 2 heard apex beat felt at 5th inter coastal space lateral to mid clavicular line no murmors
CNS examination
HIGHER MENTAL FUNCTIONS:
Conscious, coherent, cooperative
Appearence and behaviour:
Emotionally stable
Recent,immediate, remote memory intact
Speech: comprehension normal, fluency normal
CRANIAL NERVE:
All cranial nerves functions intact
SENSORY FUNCTIONS
SPINOTHALAMIC TRACT
Pain , temperature ,presure- intact in all limbs
Posterior column:
Fine touch, vibration and proprioception are intact
MOTOR SYSTEM :
Right Left
Bulk:
Inspection. N. N
Palpation. N. N
Tone:
UL. N. N
LL. N. N
REFLEXES :
B T S K A P
R + + + + + Flexor
L + + + + + Flexor
CEREBELLUM:
Finger nose Incoordination - No
Knee heel incoordination - No
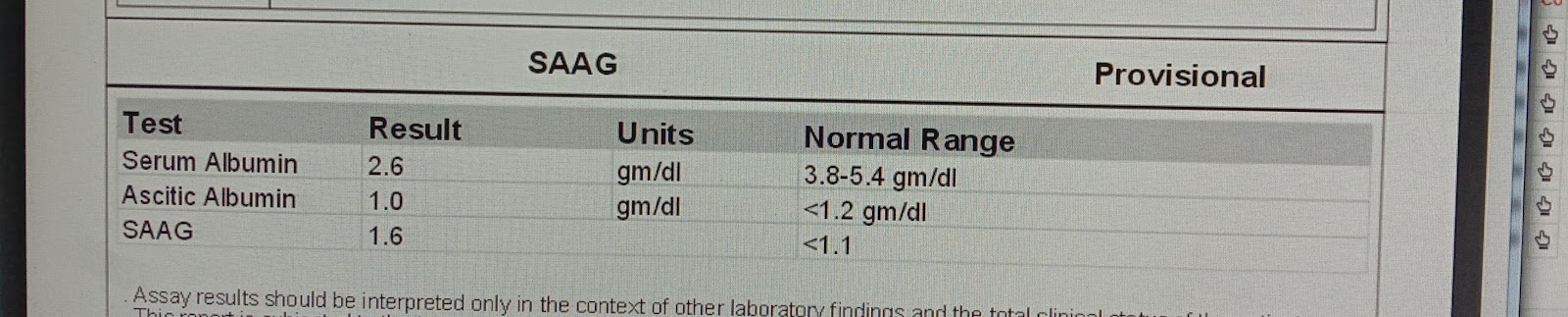
Ascitic tapping was done on 21/11/2023 night and drained about 1200 ml of ascitic fluid
Link for ascitic tapping
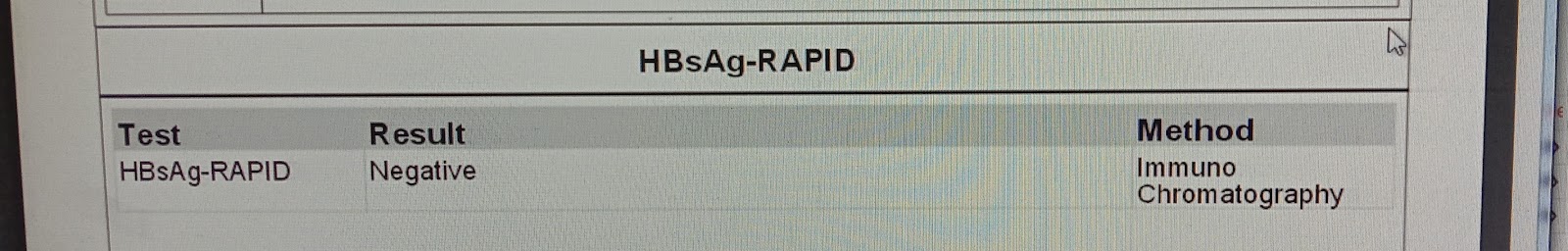
Investigations
Provisional diagnosis
Chronic liver disease with Diabetes Mellitus type II
Soap notes
S :
Rx
1) fluid restriction ‹1.5 lit/day
2) salt restriction ‹ 2 gm /day
3) INJ THIAMINE 200mg in 100 ml NS/BD
4) T. RIFAGUT 550 mg OD
5) T. UDILIV 300 mg BD
6) T. DAPAGLIFLOZIN 5 mg + T. TENLIGLIPTIN 20 MG PO BD
7) SYP LACTULOSE 15 ML TID
8) T . LASILACTONE 20/50 BD
























Comments
Post a Comment